Skin neoplasms are growths on the skin which can have many causes. The three most common skin cancers are basal cell cancer, squamous cell cancer, and melanoma, each of which is named after the type of skin cell from which it arises. Skin cancer generally develops in the epidermis (the outermost layer of skin), so a tumor is usually clearly visible. This makes most skin cancers detectable in the early stages. Unlike many other cancers, including those originating in the lung, pancreas, and stomach, only a small minority of those afflicted will actually die of the disease. In fact, though it can be disfiguring, except for melanoma, skin cancer is rarely fatal. Skin cancer represents the most commonly diagnosed cancer, surpassing lung, breasts, colorectal, and prostate cancer. Melanoma is less common than basal cell carcinoma and squamous cell carcinoma, but it is the most serious—for example, in the UK there are 9,500 new cases of melanoma each year, and 2,300 deaths. It is the most common cancer in the young population (20 – 39 age group). Most cases are caused by long periods of exposure to the sun. Non-melanoma skin cancers are the most common skin cancers. The majority of these are basal cell carcinomas. These are usually localized growths caused by excessive cumulative exposure to the sun and do not tend to spread.
What causes Skin Cancer?
Ultraviolet (UV) light exposure, most commonly from sunlight, is overwhelmingly the most frequent cause of skin cancer.
Other important causes of skin cancer include the following:
- Use of tanning booths
- Immunosuppression-impairment of the immune system, which protects the body from foreign entities, such as germs or substances that cause an allergic reaction. This may occur as a consequence of some diseases or can be due to medications prescribed to combat autoimmune diseases or prevent organ transplant rejection.
- Exposure to unusually high levels of x-rays
- Contact with certain chemicals-arsenic (miners, sheep shearers, and farmers), hydrocarbons in tar, oils, and soot (may cause squamous cell carcinoma)
The following people are at the greatest risk:
- People with fair skin, especially types that freckle, sunburn easily, or become painful in the sun
- People with light (blond or red) hair and blue or green eyes
- Those with certain genetic disorders that deplete skin pigment such as albinism, xeroderma pigmentosum
- People who have already been treated for skin cancer
- People with numerous moles, unusual moles, or large moles that were present at birth
- People with close family members who have developed skin cancer
- People who had at least one severe sunburn early in life
Basal cell carcinomas and squamous cell carcinomas are more common in older people. Melanomas are more common in younger people. For example, melanoma is the most common cancer in people 25-29 years of age.
Classification
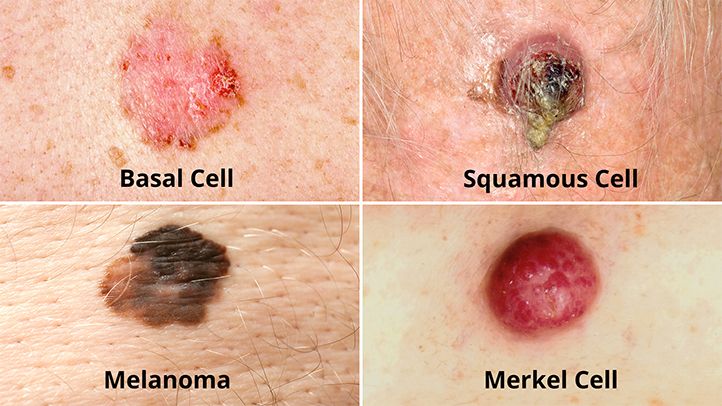
The three most common types of skin cancers are:
- Basal cell carcinoma
- Squamous cell carcinoma
- Malignant melanoma
Basal cell carcinomas are present on sun-exposed areas of the skin, especially the face. They rarely metastasize and rarely cause death. They are easily treated with surgery or radiation. Squamous cell carcinomas (SCC) are common, but much less common than basal cell cancers. They metastasize more frequently than BCCs. Even then, the metastasis rate is quite low, with the exception of SCCs of the lip, ear, and in immunosuppressed patients.
Melanomas are the least frequent of the 3 common skin cancers.
Less common skin cancers include: Dermatofibrosarcoma protuberans, Merkel cell carcinoma, Kaposi’s sarcoma, keratoacanthoma, spindle cell tumors, sebaceous carcinomas, microcystic adnexal carcinoma, Pagets’s disease of the breast, atypical fibroxanthoma, leimyosarcoma, and angiosarcoma
The BCC and the SCC often carry a UV-signature mutation indicating that these cancers are caused by UV-B radiation via the direct DNA damage. The indirect DNA damage is caused by free radicals and reactive oxygen species. Research indicates that the absorption of three sunscreen ingredients into the skin, combined with a 60-minute exposure to UV, leads to an increase of free radicals in the skin, if applied in too little quantities and too infrequently. However, the researchers add that newer creams often do not contain these specific compounds, and that the combination of other ingredients tends to retain the compounds on the surface of the skin. They also add the frequent re-application reduces the risk of radical formation.
Skin cancer as a group
The three main types of cancer are not similar and basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and malignant melanoma cannot be viewed as skin cancer.
- the mechanism that generates the first two forms is different from the mechanism that generates the melanoma. The direct DNA damage is responsible for BCC and SCC while the indirect DNA damage causes melanoma.
- the mortality rate of BCC and SCC is around 0.3% causing 2000 deaths per year in the US. In comparison the mortality rate of melanoma is 15-20% and it causes 6500 deaths per year.
Even though it is much less common than BCCs and SCCs, malignant melanoma is responsible for 75% of all skin cancer-related deaths.
While sunscreen has been shown to protect against BCC and SCC it may not protect against malignant melanoma. When sunscreen penetrates into the skin it generates reactive chemicals. It has been found that sunscreen use is correlated with malignant melanoma.
Experimental and the epidemiological evidence suggests that sunscreen use correlates with melanoma incidence. This gives rise to questions regarding the possibility that a sunscreen user’s lifetime exposure to ultraviolet light may be higher than average. Alternatively, one might question whether sun screens are themselves tumor promoters or carcinogens. Arguably, sunscreen users are the ones most likely to be burned or have been burned by sun light. Similarly, most sunscreens primarily screen UVB, the primary cause of sunburn, while UVA is the primary cause of melanoma. Thus, by limiting the discomfort of sunburn, UVB screening may indirectly result in more UVA exposure. In any case, if some sunscreens promote skin cancer, physical light-scattering sunscreens based in zinc oxide, titanium dioxide or some other natural base are likely safer than chemical blockers such as benzones, etc., as they will be less chemically active.
What are the Symptoms of Skin Cancer?
A basal cell carcinoma (BCC) usually looks like a raised, smooth, pearly bump on the sun-exposed skin of the head, neck, or shoulders.
- Small blood vessels may be visible within the tumor.
- A central depression with crusting and bleeding (ulceration) frequently develops.
- A BCC is often mistaken for a sore that does not heal.
A squamous cell carcinoma (SCC) is commonly a well-defined, red, scaling, thickened patch on sun-exposed skin.
- Like BCCs, SCCs may ulcerate and bleed.
- Left untreated, SCC may develop into a large mass.
The majority of malignant melanomas are brown to black pigmented lesions.
- Warning signs include change in size, shape, color, or elevation of a mole.
- The appearance of a new mole during adulthood, or new pain, itching, ulceration, or bleeding of an existing mole should all be checked by a health-care provider.
The following easy-to-remember guideline, “ABCD,” is useful for identifying malignant melanoma:
- Asymmetry-One side of the lesion does not look like the other.
- Border irregularity-Margins may be notched or irregular.
- Color-Melanomas are often a mixture of black, tan, brown, blue, red, or white.
- Diameter-Cancerous lesions are usually larger than 6 mm across (about the size of a pencil eraser), but any change in size may be significant.
Diagnosis
If you have a worrisome mole or other lesion, your primary-care provider will probably refer you to a dermatologist. The dermatologist will examine any moles in question and, in many cases, the entire skin surface.
- Any lesions that are difficult to identify, or are thought to be skin cancer, may then be checked.
- A sample of skin (biopsy) will be taken so that the suspicious area of skin can be examined under a microscope.
- A biopsy can almost always be done in the dermatologist’s office.
If a biopsy shows that you have malignant melanoma, you will probably undergo further testing to determine the extent of spread of the disease, if any. This may involve blood tests, a chest x-ray, and other tests as needed.
Methods of Treatment
Treatment is dependent on type of cancer, location of the cancer, age of the patient, and whether the cancer is primary or a recurrence. One should look at the specific type of skin cancer (basal cell carcinoma, squamous cell carcinoma, or melanoma) of concern in order to determine the correct treatment required. An example would be a small basal cell cancer on the cheek of a young man, where the treatment with the best cure rate (Mohs surgery or CCPDMA) might be indicated. In the case of an elderly frail man with multiple complicating medical problems, a difficult to excise basal cell cancer of the nose might warrant radiation therapy (slightly lower cure rate) or no treatment at all. Topical chemotherapy might be indicated for large superficial basal cell carcinoma for good cosmetic outcome, whereas it might be inadequate for invasive nodular basal cell carcinoma or invasive squamous cell carcinoma. In general, melanoma is poorly responsive to radiation or chemotherapy.
For low-risk disease, radiation therapy (external beam radiotherapy or brachytherapy), topical chemotherapy (imiquimod or 5-fluorouracil) and cryotherapy (freezing the cancer off) can provide adequate control of the disease; both, however, may have lower overall cure rates than certain type of surgery. Other modalities of treatment such as photodynamic therapy, topical chemotherapy, electrodessication and curettage can be found in the discussions of basal cell carcinoma and squamous cell carcinoma.
Mohs’ micrographic surgery (Mohs surgery) is a technique used to remove the cancer with the least amount of surrounding tissue and the edges are checked immediately to see if tumor is found. This provides the opportunity to remove the least amount of tissue and provide the best cosmetically favorable results. This is especially important for areas where excess skin is limited, such as the face. Cure rates are equivalent to wide excision. Special training is required to perform this technique. An alternative method is CCPDMA and can be performed by a pathologist not familiar with Mohs surgery.
In the case of disease that has spread (metastasized), further surgical procedures or chemotherapy may be required.
Scientists have recently been conducting experiments on what they have termed “immune- priming”. This therapy is still in its infancy but has been shown to effectively attack foreign threats like viruses and also latch onto and attack skin cancers. More recently researchers have focused their efforts on strengthening the body’s own naturally produced “helper T cells” that identify and lock onto cancer cells and help guide the killer cells to the cancer. Researchers infused patients with roughly 5 billion of the helper T cells without any harsh drugs or chemotherapy. This type of treatment if shown to be effective has no side effects and could change the way cancer patients are treated.
A cream used to treat pre-cancerous skin lesions also reverses signs of aging, a study released in April 2009 indicated. In March 2010 academics from Dundee University in Scotland announced they had devised a new, less-painful method of treating skin cancer, which could be administered from the home.
Post surgery reconstruction
Currently, surgical excision is the most common form of treatment for skin cancers. The goal of reconstructive surgery is restoration of normal appearance and function. The choice of technique in reconstruction is dictated by the size and location of the defect. Excision and reconstruction of facial skin cancers is generally more challenging due to presence of highly visible and functional anatomic structures in the face.
When skin defects are small in size, most can be repaired with simple repair where skin edges are approximated and closed with sutures. This will result in a linear scar. If the repair is made along a natural skin fold or wrinkle line, the scar will be hardly visible. Larger defects may require repair with a skin graft, local skin flap, pedicled skin flap, or a microvascular free flap. Skin grafts and local skin flaps are by far more common than the other listed choices.
Skin grafting is patching of a defect with skin that is removed from another site in the body. The skin graft is sutured to the edges of the defect, and a bolster is placed atop the graft for seven to ten days, to immobilize the graft as it heals in place. There are two forms of skin grafting: split thickness and full thickness. In a split thickness skin graft, a shaver is used to shave a layer of skin from the abdomen or thigh. The donor site, regenerates skin and heals over a period of two weeks. In a full thickness skin graft, a segment of skin is totally removed and the donor site needs to be sutured closed. Split thickness grafts can be used to repair larger defects, but the grafts are inferior in their cosmetic appearance. Full thickness skin grafts are more acceptable cosmetically. However, full thickness grafts can only be used for small or moderate sized defects.
Local skin flaps are a method of closing defects with tissue that closely matches the defect in color and quality. Skin from the periphery of the defect site is mobilized and repositioned to fill the deficit. Various forms of local flaps can be designed to minimize disruption to surrounding tissues and maximize cosmetic outcome of the reconstruction. Pedicled skin flaps are a method of transferring skin with an intact blood supply from a nearby region of the body. An example of such reconstruction is a pedicled forehead flap for repair of a large nasal skin defect. Once the flap develops a source of blood supply form its new bed, the vascular pedicle can be detached.
Drugs rating:
| Title | Votes | Rating | ||
| 1 | Carac Cream (Fluorouracil) | 1 |
|
(10.0/10) |
| 2 | Efudex Cream (Fluorouracil) | 13 |
|
(7.4/10) |
| 3 | Methotrexate | 231 |
|
(6.5/10) |
| 4 | Fluoroplex Cream (Fluorouracil) | 1 |
|
(1.0/10) |
| 5 | Trexall (Methotrexate) | 0 |
|
(0/10) |
Follow-up
Most skin cancer is cured surgically in the dermatologist’s office. Of skin cancers that do recur, most do so within three years. Therefore, follow up with your dermatologist (skin specialist) as recommended. Make an appointment immediately if you suspect a problem.
If you have advanced malignant melanoma, your oncologist may want to see you every few months. These visits may include total body skin examinations, regional lymph node checks, and periodic chest x-rays. Over time, the intervals between follow-up appointments will increase. Eventually these checks may be done only once a year.
Prevention
Although it is impossible to completely eliminate the possibility of skin cancer, the risk of developing such a cancer can be reduced significantly with the following steps:
- Avoid the use of tobacco products.
- Reducing overexposure to ultraviolet (UV) radiation, especially in early years
- Avoiding sun exposure during the peak UV times during the day, typically from 10 AM to 3 PM (dependent on country) when the sun is directly overhead
- Wearing protective clothing (long sleeves and hats) when outdoors
- Using a broad-spectrum sunscreen that blocks both UVA and UVB radiation
- Reapply sun block as per the manufacturers directions
Australian scientist Ian Frazer who developed a vaccine for cervical cancer, says that a vaccine effective in preventing for certain types of skin cancer has proven effective on animals and could be available within a decade. The vaccine would only be effective against Squamous Cell Carcinoma.
Primary health care providers should examine their patients during the course of a routine comprehensive physical examination by means of a full body screening (all areas of the body’s skin surface are examined, with the use of a special light and a magnifying glass, for abnormal masses, lesions, and cancerous neoplasms like BCC, SCC, and MM). Referrals or visits to a dermatologist will usually include this as a first part of the examination. Many times, hospitals, doctor’s offices, and dermatologist’s offices will perform these for the general public as part of a mass screening program done at certain times during the year, and these are usually free or are low-priced and thus are often very popular. If necessary, skin cells from the outer epidermis can be scraped off or an actual biopsy performed, and the results examined for pathologies.